ECG INSIGHTS
Dr. Santhosh K R,
Senior Consultant, Dept. of Cardiology, PRS Hospital
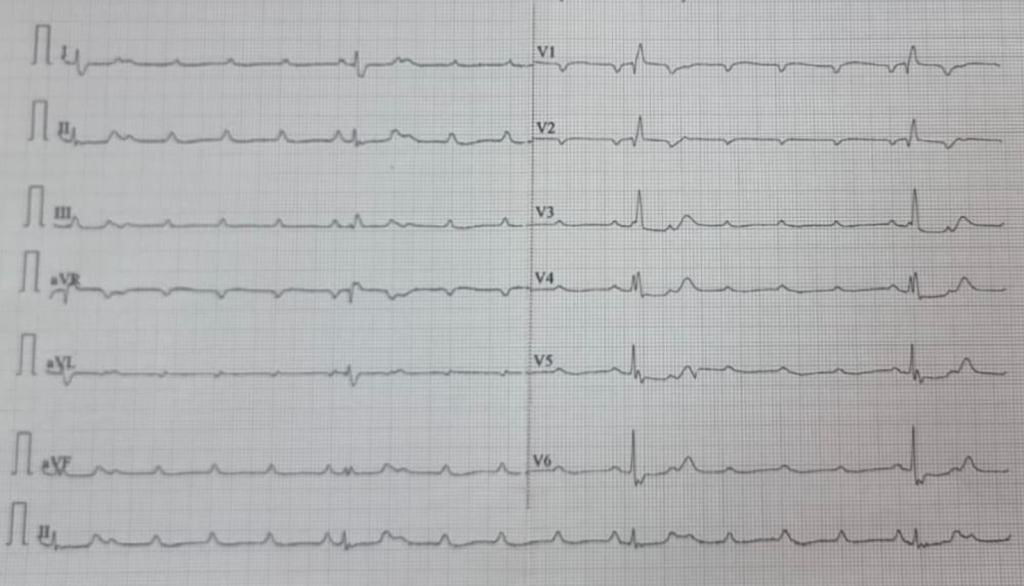
This is the E.C.G of a 69 year old male who presented to the casualty with history of one episode of seizures followed by loss of consciousness which lasted for few seconds.
What is the E.C.G diagnosis?
How will you proceed to treat this patient?
E.C.G shows extreme bradycardia with heart rate around 20/mt. There are regular P waves coming at a rate of 100/mt. QRS has a Right Bundle Branch Block morphology with a rate around 20/mt. There is no relationship with P and QRS. So E.C.G shows complete heart block (C.H.B).
Can you make out anything else from E.C.G?
If you look carefully you can see 1 mm ST depression in II, III, aVF, V5, V6. This might give you a clue regarding archeology of complete heart block (C.H.B).
Differential diagnoses that should come to your mind is degenerative C.H.B or an acute coronary syndrome (A.C.S). Degenerative CHB occurs in elderly people and can have a similar presentation. But in this patient because of ST depression in E.C.G one should think of associated coronary artery disease (C.A.D). Here history becomes important. Our aim should be to clarify whether patient has possible CAD. The most important thing would be history of chest discomfort or pain proceeding the seizures. Since the patient had come to the hospital within one hour of symptoms, doing a cardiac marker like Troponin estimation may not be helpful at this point. Usually C.H.B occurs in a patient with acute inferior wall ST elevation myocardial infarction. In our patient detailed enquiry denied any sort of chest discomfort prior to this episode.
The treatment for a degenerative C.H.B would be to convert the temporary pacing to a permanent pacing. But in this particular case because patient had risk factors for C.A.D like diabetes, hypertension and dyslipidemia and suspicious ST depression in E.C.G, one should definitely rule out acute coronary syndrome prior to proceeding with permanent pacemaker implantation.
Hence patient was shifted to the cardiac catheterization laboratory, a temporary transvenous pacing was done through the right femoral vein and a coronary angiogram (C.A.G) was done through right femoral artery. CAG showed a totally occluded proximal right coronary artery (R.C.A) which was tackled with primary angioplasty with stent implantation in RCA. Immediately after the procedure, patient attained sinus rhythm with a heart rate of 100/mt and was stable hemodynamically and temporary pacemaker could be removed.
This E.C. G was shown to illustrate the fact that one should not been carried away by the obvious findings, but look for subtle findings which will help you to come to a proper treatment plaeet


